For millions of parents, the journey with childhood eczema begins the same way: a small patch of dry, irritated skin appears, then spreads—and can lead to sleepless nights, constant scratching, stress for both parents and children, and persistent questions about what's happening beneath the surface.
Childhood eczema affects roughly 1 in 10 children in the United States, with many experiencing their first flare before their first birthday. Emerging research highlights a crucial but often overlooked factor: the skin’s microbiome, the ecosystem of microorganisms that help protect and regulate the skin.
Why Infant Skin Is More Vulnerable to Eczema
Infant skin is fundamentally different from adult skin. First, babies have a thinner skin barrier, produce less natural oil, and lose moisture more quickly. Second, their immune system is still developing and can be more reactive to irritants. Third, their skin microbiome—the beneficial and potentially harmful bacteria living on the skin's surface—is also still developing. All of these factors make young skin more vulnerable to imbalance, irritation, and eczema flares.
“The severity of a child's eczema often correlates directly with the level of Staph aureus. By targeting this bacterial imbalance—rather than simply suppressing symptoms—families and healthcare providers can work together to restore the skin's natural defenses."
The Microbiome Connection: How Staph Aureus Bacteria Drives Flares
"A dysfunctional skin barrier is central to atopic dermatitis and, importantly, opens the door for an imbalanced microbiome,” says Peter Lio, MD, Clinical Assistant Professor of Dermatology & Pediatrics at Northwestern University. “That, in turn, allows for Staph aureus to dominate and release toxins that further damage the skin barrier, resulting in a vicious cycle of disease that can be very difficult to break."
During active eczema flares, Staph aureus bacteria takes over the beneficial microbiome: Present in up to 90% of flare-ups, this harmful bacteria releases toxins that trigger inflammation and weaken the barrier further.
"When we look at pediatric eczema through the lens of the microbiome, we see a different picture,” explains Jeff Yu, MD, Chair of Dermatology at Virginia Commonwealth University. “The severity of a child's eczema often correlates directly with the level of Staph aureus. By targeting this bacterial imbalance—rather than simply suppressing symptoms—families and healthcare providers can work together to restore the skin's natural defenses."
Common Eczema Triggers in Babies and Toddlers
Common childhood eczema triggers include:
- Hot baths
- Harsh or fragranced cleansers
- Dyes or fragrances in laundry detergents
- Wool or synthetic fabrics
- Dry indoor heat, cold weather, or low humidity
- Saliva during teething
- Possible food sensitivities (consult a pediatrician)
Your Childhood Eczema Care Strategy: A Step by Step Guide
1. Microbiome-Restorative Care
Traditional eczema care focuses on managing symptoms. The patented TPZ-01™ enzyme used in hypothesis™ formulas is designed to target Staph aureus while preserving beneficial bacteria—addressing the root cause, not just the irritation.
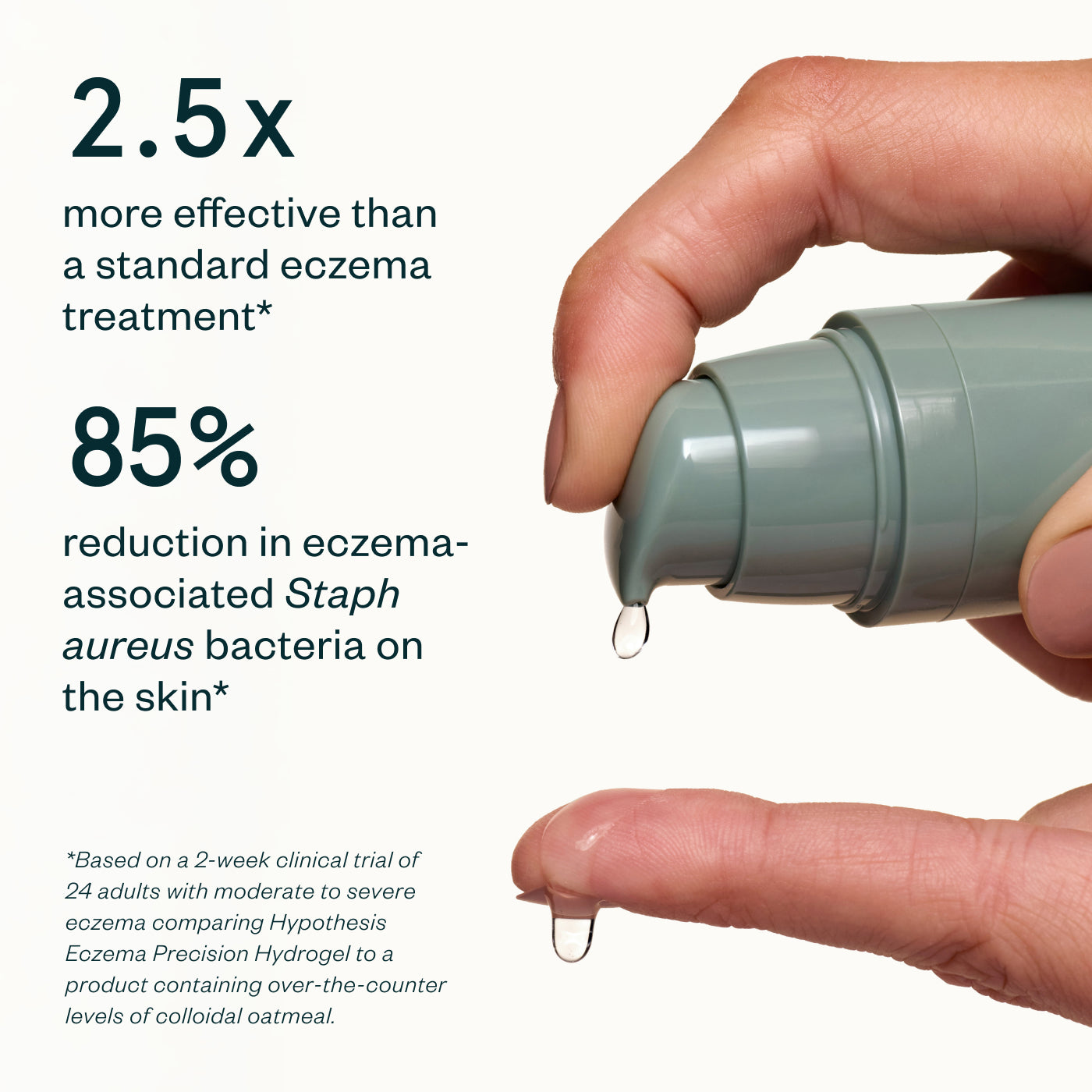
- Eczema Precision Hydrogel: Our lightweight, cooling gel targets flares directly at the source. Powered by TPZ-01™ enzyme to eliminate eczema-causing Staph aureus bacteria, plus colloidal oatmeal and Vitamin B5 for hydration and barrier repair. The fast-absorbing formula delivers real, lasting relief for eczema-prone skin.
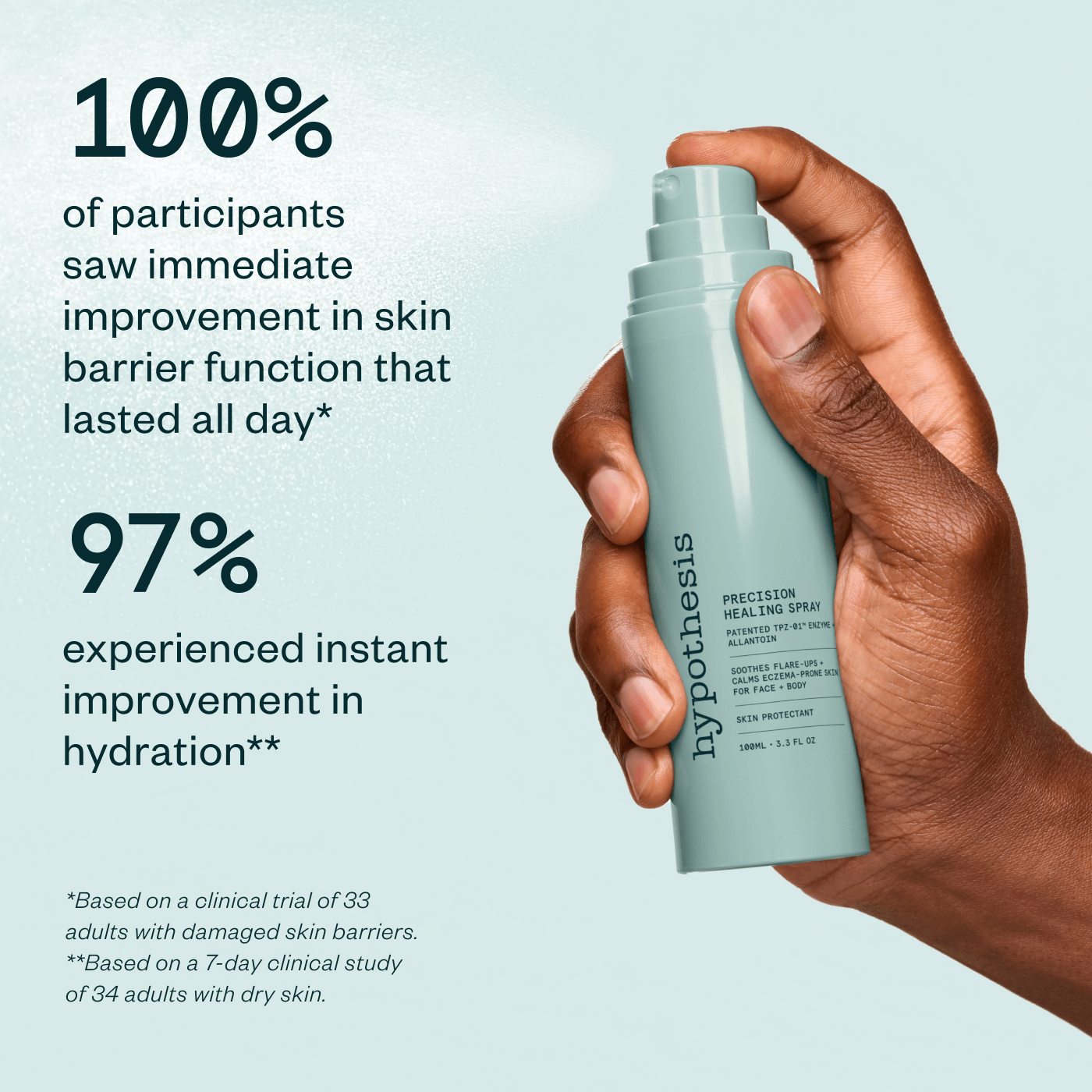
- Precision Healing Spray: An extra-fine, no-touch spray that targets eczema-causing bacteria in hard-to-reach areas, and is perfect for active children or quick application between diaper changes. The TPZ-01™ enzyme resets the skin's microbiome balance while allantoin and Vitamin B5 calm irritation. It’s also ideal for on-the-go relief and fits neatly into diaper bags.
2. Barrier-Supportive Moisture
After addressing bacterial imbalance, the next step is locking in hydration and strengthening the barrier. Look for fragrance-free moisturizers with ceramides, cholesterol, fatty acids, hyaluronic acid, or glycerin—all ingredients that support the lipid matrix and provide lasting moisture.
- Eczema Therapy Cream: Formulated to work in parallel with TPZ-01™ products, our deeply soothing moisturizer seals in results and is perfect for replenishing children’s developing skin barriers. Three essential ceramides restore the lipid matrix, while colloidal oatmeal and bisabolol stop the itch and calm redness.
Apply Eczema Therapy Cream after Eczema Precision Hydrogel or Precision Healing Spray as part of a comprehensive eczema-soothing regimen. All three hypothesis™products are dermatologist tested and certified safe and effective for all ages, with four independent certifications: EWG Verified®, National Eczema Association Seal of Acceptance™, MyMicrobiome Microbiome-Friendly for infants and adults, and Leaping Bunny Certified. All formulas are also fragrance-free, steroid-free, and safe for use around the eyes.
3. Bath Time Strategies for Babies and Toddlers
Bath time can either soothe or trigger eczema. Use lukewarm water (test with your elbow—it should feel warm, not hot) and keep baths to 5-10 minutes. Choose fragrance-free, pH-balanced cleansers around 5.5. For younger babies, plain water often works for most baths, using cleanser only where needed in spots like the diaper area.
Pat dry with a soft towel, leaving skin a little damp. Apply moisturizer within 3 minutes using the “soak and seal” method—this window is critical since moisture evaporates extra-quickly from infant skin.
4. Managing Their Environment
Drool and teething: Keep a soft cloth handy to gently pat excess saliva around the mouth and chin. Apply Eczema Therapy Cream as a protective barrier after feeding.
Comfortable clothing: Babies and toddlers are constantly crawling, rolling, and reaching. Dress them in loose-fitting, 100% cotton clothing and check that seams and elastic aren't rubbing eczema-prone areas like the neck, wrists, and diaper area.
Temperature during play: Active toddlers overheat easily, triggering itching. Dress them in breathable layers you can remove and keep playrooms cool (65-68°F). Use a humidifier to keep indoor humidity around 40-50% to prevent moisture loss.
Bedding and laundry: Use fragrance-free, dye-free laundry detergent with an extra rinse cycle for baby clothes and bedding.
5. Adapting Care as Your Child Grows
Childhood eczema changes with development. What works at 6 months may need some tweaking by 18 months.
Try tracking your child’s flare patterns along with developmental milestones: growth spurts, teething, starting solids, beginning daycare, or illness can temporarily destabilize the microbiome. This helps you anticipate and prevent flares rather than just reacting.
Work closely with your pediatrician. Schedule regular check-ins to discuss whether your approach is keeping up with your child's development, not just when flares worsen.
Managing Childhood Eczema Long-Term
Childhood eczema is more than dry skin; it has to do with genetics, environment, barrier function, and microbial balance. A microbiome-supportive routine, combined with consistency and pediatric guidance, can help families maintain calmer, more predictable skin—and fewer sleepless nights.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your child's pediatrician or dermatologist for diagnosis and treatment.